Scabies is a highly infectious skin infestation caused by tiny mites that burrow into the outer layer of the skin. It causes severe itching and a characteristic rash, with symptoms typically worsening at night. Although anyone can become infected, scabies spreads more easily in crowded settings where many people share the same physical space. The infestation can take months to fully treat, while it can spread to others very quickly. Early diagnosis and management are essential to prevent transmission.
Key Takeaways
- Scabies spreads through prolonged skin-to-skin contact and causes intense nighttime itching.
- Rash and burrows often appear on the hands, wrists, waistline, and genital area.
- Diagnosis is clinical and may be confirmed with a skin scraping.
- Treatment requires prescription medications and simultaneous care for all close contacts.
What is Scabies?
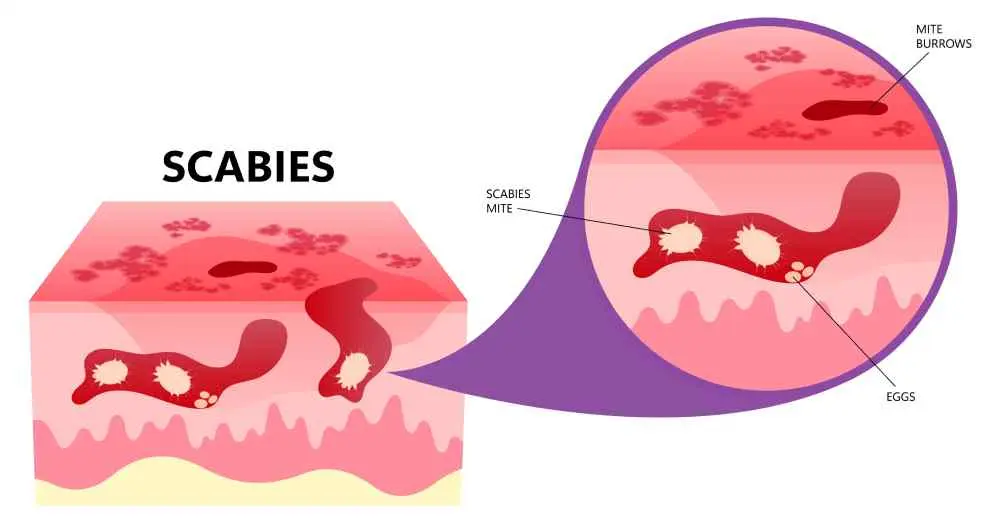
Scabies is a skin infestation caused by the mite Sarcoptes scabiei, which burrows under the surface of the skin to deposit its eggs. This triggers an allergic reaction that leads to intense itching and a characteristic rash. The infestation spreads easily and must be treated with prescription medication to kill the mites. It is not related to poor hygiene and can affect people of any age or background.
How Scabies Spreads
Scabies is mostly transmitted by close and long duration of skin-to-skin contact with an infected individual. It may also be passed by way of sharing items but this is less widespread. The mites do not jump or fly and therefore the transmission needs sustained contact. Poor living conditions enhance the spread.
Scabies spreads through:
- Prolonged physical contact with a host person
- Sexually sharing bedding, towels or clothes
- Physical contact with people having the crusted scabies, which is extremely contagious
Scabies Symptoms
These symptoms are caused by the allergicity of the body to the mites, their eggs, and their garbage. Itching is likely to increase at night and can impair sleep. A scabies rash may be mistaken with other skin-related diseases and hence proper diagnosis is crucial. The symptoms are normally observed 2-6 weeks following the first contact.
Typical symptoms include:
- Intense nighttime itching
- Bumps or pimples on the skin that are small and reddish
- Wavy burrow lines on the skin surface that are thin
- Scratching, blisters, crusting, or sores
- Diffuse rash is present in severe or untreated cases
Where Scabies Rash Typically Appears
The scabies rash may occur in any part of the body although the mites prefer warm and thin skin. Distribution pattern will enable the identification of scabies and other skin diseases.
The most frequent places of the common rash are:
- Finger webs and wrists
- Armpits, waistline, elbows
- Buttocks and genital region
- Breasts and shoulder blades
- In infants: head, face, neck, palms and soles
How Scabies Is Diagnosed
It is diagnosed using clinical assessment, pattern of the symptoms, and distribution of the rash. Scabies can be diagnosed by a medical worker through the detection of mites or eggs. Itching and rash may be similar to eczema, allergies and thus proper examination is essential.
Diagnostic methods include:
- Rash and burrow are examined visually
- Skipping the skin to find mites, eggs or fecal balls with a microscope
- Magnification to study burrows by means of dermatoscopy
- Checking the recent exposure history and symptoms
Scabies Treatments
Treatment goes to destroy mites and avoid reinfestation. The principal mode of therapy is prescription topical medications, and close contacts should be treated at the same time. The itching can be persistent several weeks following the killing of mites because of persistent skin irritation.
The standard treatment options are:
- Antihistamines or itch relievers lotions
- Sexual contacts and household members treated simultaneously
- Laundering of clothing, bedding and towels that were used in the past
How to Prevent Scabies Transmission
It is necessary to prevent the transmission by medical treatment and environmental cleaning. Mites do not last long off the body so decontamination will minimize the possibility of reinfestation. Practice at an early stage within the household and institutes restrains outbreaks.
Preventive strategies are:
- Skin-to-skin contacts with the infested to be avoided
- Infecting all close acquaintances at the same time
- Laundering of bedding, towels and clothing using hot water and high heat on the dryer
- Putting unwashable things into bags and leaving them there over a few days
- Washing living quarters, furniture and areas that are touched so often.
Scabies in Children and Infants
In young children and infants, scabies does not always present in the same way. The rash may also involve the face, scalp, neck, palms, and soles—areas not typically affected in adults. Itching may lead to sleep disturbances and feeding problems. Diagnosis should be made carefully, and treatment must follow pediatric guidelines. Treatment should also be given to all caregivers and household members to prevent rapid reinfestation.

Scabies Risk Factors
Some settings and circumstances predispose to scabies. The infestation is often widespread where a prolonged contact or a close form of living is prevalent. Severe forms are also more prone to the immunocompromised individuals.
Key risk factors include:
- Residing in congested areas
- Intimate contact with an infected individual
- Using communal bedding, clothing or towels
- Weakened immune system
- Old age or long-term care centers
This content is for informational purposes only and is not a substitute for medical advice. If you’re experiencing any of these symptoms, please contact us for professional help.
Frequently Asked Questions About Scabies
What is the fastest way to cure scabies?
The quickest and most efficient remedy is by treating all the close people simultaneously with a prescribed medication like permethrin cream or oral ivermectin. Reinfestation is avoided through cleaning the environment.
How does a person get scabies?
When a person has prolonged contact with someone with scabies, he or she contract the disease. It is also rare to be transmitted via shared bedding or clothing.
How do I test myself for scabies?
Self testing cannot be relied upon, as symptoms may be similar to other diseases. Due to the need to diagnose scabies, the clinician will have to examine the skin and, possibly, a skin scraping.
What are the first signs of scabies?
The first symptoms include what appear as tiny red spots that have strange burrows on the skin, and itch intensely during the night time.
What is commonly mistaken for scabies?
Common skin infections mistaken with scabies are eczema, dermatitis, allergic reactions and bedbug bites because their itching is similar, as well as the patterns of rashes.
Which doctor should be consulted for scabies?
For the treatment of scabies, the Dermatology Department should be consulted.

 Let Us Call You
Let Us Call You
































