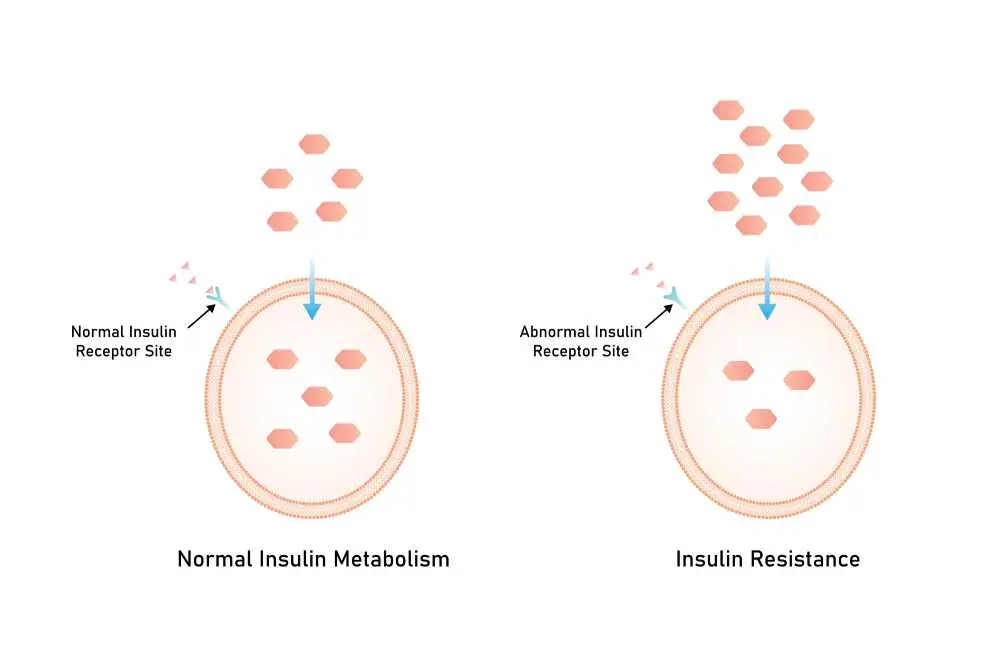
Insulin Resistance is a complex physiological state where the body's cells in the muscles, fat, and liver do not respond properly to insulin and cannot easily take up glucose from the blood. As a result, the pancreas produces more insulin to help glucose enter the cells. Over time, the pancreas can no longer keep up with the increased demand, leading to elevated blood sugar levels. Understanding this condition is the first step toward preventing the onset of type 2 diabetes and other metabolic complications.
What is Insulin Resistance?
The insulin resistance meaning describes a condition where the "key" (insulin) fails to open the "locks" (cell receptors) efficiently, causing sugar to build up in the bloodstream. While the body initially compensates by overproducing insulin a state known as hyperinsulinemia this cycle can eventually exhaust the pancreas. This metabolic inefficiency is often a precursor to prediabetes and is a central component of metabolic syndrome.
What Causes Insulin Resistance?
The meaning of insulin resistance in a biological context is often rooted in a combination of genetic factors and lifestyle triggers like excess body fat. Specifically, visceral fat around the organs secretes inflammatory substances that interfere with insulin signaling. Other primary causes include:
- Physical ınactivity
- High-calorie diets
- Hormonal ımbalances
- Sleep deprivation
Insulin Resistance Symptoms
Typical insulin resistance symptoms are often silent in the early stages, meaning many individuals are unaware of the condition until blood sugar levels reach a critical point. However, as the body struggles to maintain balance, some people may experience specific physical changes:
- Increased hunger
- Lethargy
- Frequent urination
- Excessive thirst
Signs Of Insulin Resistance
Visible signs of insulin resistance can serve as important clinical clues during a physical examination. These indicators often manifest on the skin or through body composition changes:
- Acanthosis Nigricans: Dark, velvety patches of skin typically found on the neck, armpits, or groin.
- Skin Tags: Small growths of skin often appearing in the neck and shoulder area.
- Abdominal Obesity: A waist measurement of over 40 inches for men or 35 inches for women.
- Slow Healing: Minor cuts or bruises taking longer than usual to resolve.
Insulin Resistance Diagnostic Methods
A clinical insulin resistance test usually involves blood work to measure fasting glucose and insulin levels simultaneously. Doctors often use the HOMA-IR (Homeostatic Model Assessment for Insulin Resistance) calculation to determine the severity of the resistance. Other diagnostic tools include the A1C test, which measures average blood sugar over three months, and the Glucose Tolerance Test, which observes how the body handles a concentrated sugar load.
Insulin Resistance Treatment
Effective insulin resistance treatment focuses on restoring the body’s sensitivity to insulin through targeted lifestyle interventions and, in some cases, medication. Most healthcare providers prioritize non-pharmacological approaches as the first line of defense. Core treatment strategies include:
- Aerobic activity and strength training both significantly increase glucose uptake by muscles.
- Focusing on whole foods, fiber, and healthy fats while reducing refined carbohydrates.
- Losing even a small percentage of body weight can drastically improve insulin function.
- A medication commonly prescribed to help the liver produce less glucose and increase cell sensitivity.
This content is for informational purposes only and is not a substitute for medical advice.
If you’re experiencing any of these symptoms, please contact us for professional help.
Which medical department should be consulted for Insulin Resistance?
Patients should consult the Endocrinology department, as these specialists focus on hormone-related disorders and the metabolic systems governing blood sugar.

 Let Us Call You
Let Us Call You

























