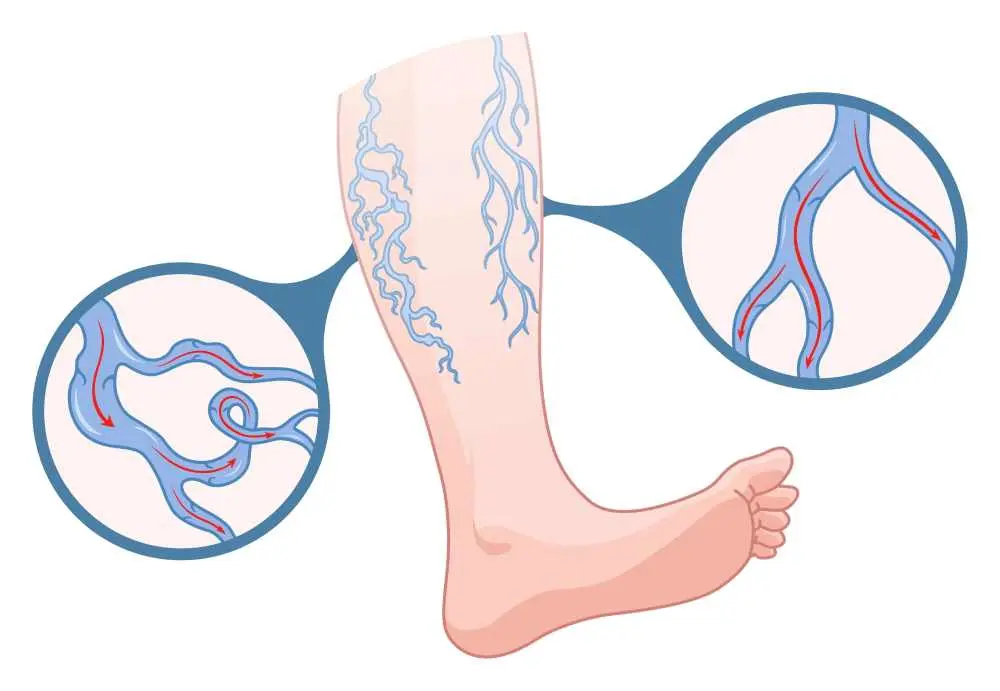
Varicose veins are swollen, twisted blood vessels that usually appear blue or dark purple and typically develop on the legs and feet. This condition occurs when the valves in the veins do not work properly, causing blood to pool or flow backward instead of toward the heart. While many people view them as a cosmetic concern, they can lead to significant discomfort and more serious circulatory issues if left untreated. Understanding the nature of this vascular condition is the first step toward effective management and long-term relief.
What are Varicose Veins?
The presence of varicose vein diseases indicates that the venous system is struggling to return blood from the lower extremities back to the heart against the force of gravity. In a healthy vein, one-way valves open to let blood through and then close to prevent it from flowing backward. When these valves become weak or damaged, blood collects in the vein, causing it to stretch, bulge, and take on the characteristic gnarled appearance.
What Causes Varicose Veins?
There are several varicose veins causes, but the most common factor is the weakening of vein walls and valves over time.
- Age: Veins lose elasticity with age, causing the valves to become weak.
- Pregnancy: Increased blood volume and hormonal changes put extra pressure on leg veins.
- Gender: Hormonal fluctuations in women (menopause, puberty) can relax vein walls.
- Family History: If other family members had the condition, your risk is significantly higher.
- Obesity: Excess weight adds significant pressure to the veins.
- Prolonged Standing or Sitting: Staying in one position for too long hinders efficient blood circulation.
Varicose Veins Symptoms
Recognizing varicose veins symptoms is essential, as the condition often starts with a dull ache or a feeling of heaviness in the legs after long periods of standing.
- A persistent, heavy, or uncomfortable feeling in the legs.
- Sensation of heat or rhythmic pulsing in the lower limbs.
- Sudden, painful contractions, especially during the night.
- Fluid buildup around the ankles and feet.
- Persistent irritation or a rash near the affected veins.
Signs Of Varicose Veins
Physical signs of varicose veins are usually quite obvious and include veins that are dark purple or blue in color. Beyond the color change, these vessels often manifest through several distinct physical indicators:
- Rope-like Appearance: Veins that appear twisted, swollen, and bulging, often resembling raised cords along the surface of the legs.
- Skin Discoloration: Reddish or brownish patches (hyperpigmentation) typically appearing near the ankles due to blood leaking into surrounding tissue.
- Texture Changes: Skin that becomes abnormally shiny, dry, thin, or scaly, which may eventually lead to a leathery texture known as lipodermatosclerosis.
- Spider Vein Clusters: The presence of smaller red or blue "webs" (telangiectasia) that often surround or precede larger varicose formations.
- Visible Swelling (Oedema): Objective swelling in the lower legs and ankles that often worsens toward the end of the day and improves after elevation.
- Venous Ulcers: Open sores or wounds that form near the ankles, often starting as a small discolored spot that fails to heal.
Varicose Veins Diagnostic Methods
The identification of varicose veins causes and the extent of the damage typically begins with a physical exam where the doctor inspects the legs while the patient is standing.
- Duplex Ultrasound: A non-invasive test that uses sound waves to check blood flow and the structure of the leg veins.
- Physical Examination: Visual inspection to look for swelling, skin changes, and the degree of bulging.
- Color Flow Imaging: Provides a visual map of the blood's speed and direction within the vessels.
- Venogram: A specialized X-ray where dye is injected to provide a detailed view of the blood vessels.
Varicose Veins Treatment
A successful varicose veins treatment plan usually begins with conservative self-care measures like wearing compression stockings and exercising regularly. Compression stockings work by squeezing the legs, helping the veins and leg muscles move blood more efficiently.
Doctors also recommend elevating the legs above the heart several times a day to reduce pressure. If lifestyle changes do not provide enough relief, sclerotherapy may be used, where a solution is injected into the vein to scar and close it, eventually causing the vein to fade.
Varicose Vein Surgery
In more advanced cases, varicose vein surgery or minimally invasive thermal procedures may be required to permanently close or remove problematic vessels. Endovenous laser treatment (EVLT) or radiofrequency ablation uses heat to seal the affected vein from the inside.
For very large or surface-level veins, a surgeon may perform ambulatory phlebectomy, which involves removing the veins through tiny skin punctures. Another traditional method is vein stripping, where the vein is physically tied off and removed through small incisions, though this is less common today due to newer, less invasive technologies.
Frequently Asked Questions About Varicose Veins
How to get rid of varicose veins in legs?
You can manage them through lifestyle changes like exercise and compression stockings, or remove them permanently with procedures like laser therapy, sclerotherapy, or surgery.
What is the main cause of varicose veins?
The primary cause is weakened or damaged valves in the veins that fail to prevent blood from flowing backward, leading to pooling and vessel stretching.
When should you worry about varicose veins?
You should seek medical attention if the veins become painful, red, or warm to the touch, or if you develop skin ulcers or bleeding near the veins
How harmful are varicose veins?
While often just a cosmetic issue, they can lead to chronic swelling, skin changes, and in some cases, the development of blood clots or open sores.
Are varicose veins dangerous?
They are generally not life-threatening, but they can increase the risk of deep vein thrombosis (DVT) or severe skin infections if the underlying circulation issue is ignored.
Which medical department should be consulted for Varicose Veins?
For varicose veins, patients should consult the Cardiovascular Surgery department. Specialists in this field evaluate venous circulation and plan appropriate diagnostic and treatment approaches based on the clinical findings.

 Let Us Call You
Let Us Call You































