Osteoarthritis is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage that cushions the ends of the bones wears down over time. Although it can damage any joint, the disorder most commonly affects joints in your hands, knees, hips, and spine. While the damage to joints cannot be reversed, symptoms can usually be managed with a combination of lifestyle changes, physical therapies, and medical interventions.
What is Osteoarthritis?
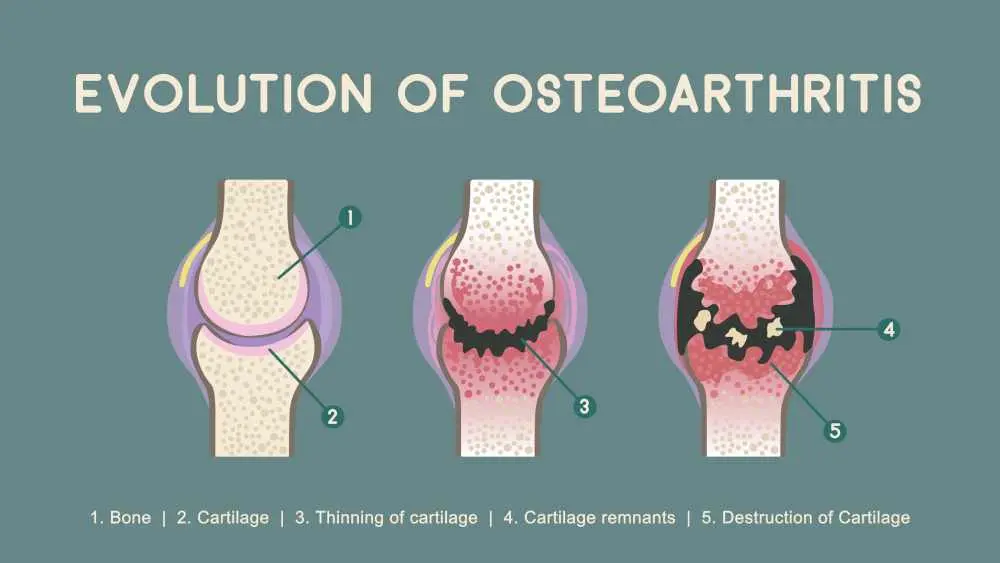
The osteoarthritis definition refers to a degenerative joint disease characterized by the breakdown of joint cartilage and underlying bone. This condition causes the bones to rub together, leading to pain, swelling, and reduced motion.
The osteoarthritis meaning is often described as "wear and tear" arthritis because it typically develops gradually as people age. Understanding this osteoarthritis disease is crucial for early intervention, as it is a leading cause of disability among older adults.
What Causes Osteoarthritis?
A primary osteoarthritis knee cause is the cumulative stress placed on the joint over years of movement and weight-bearing activities.
- Aging
- Joint ınjuries
- Obesity
- Genetics
- Bone deformities
What Are The 4 Stages Of Osteoarthritis?
In cases of knee osteoarthritis, doctors generally categorize the progression of the disease into four distinct stages based on severity.
Stage 1: Minor
During this initial stage, there is very minor wear and tear and small bone spur growths, but the patient usually experiences little to no pain.
Stage 2: Mild
This stage is considered mild, where bone spurs are more noticeable on X-rays and the space between bones begins to narrow, causing occasional stiffness or pain.
Stage 3: Moderate
In the moderate stage, the cartilage shows obvious damage and the gap between the bones narrows significantly, leading to frequent pain during daily activities.
Stage 4: Severe
The most advanced stage involves the complete loss of cartilage in the joint space, resulting in a "bone-on-bone" condition that causes intense pain and major mobility issues.
Osteoarthritis Symptoms
The most prevalent osteoarthritis symptoms include joint pain and stiffness that are often most noticeable upon awakening or after a period of inactivity.
- Affected joints might hurt during or after movement.
- Joint stiffness might be most noticeable upon awakening or after being inactive.
- Your joint might feel tender when you apply light pressure to or near it.
- You might not be able to move your joint through its full range of motion.
- You might feel or hear a popping or crackling sound when you use the joint.
Signs Of Osteoarthritis
When evaluating osteoarthritis knee osteoarthritis progression, clinicians look for visible signs such as swelling or bony enlargements in the joint area.
- Joint Swelling: Inflammation of the soft tissue or excess fluid accumulation around the joint.
- Bony Enlargements: Visible or palpable lumps, such as Heberden's nodes on the finger joints.
- Muscle Weakness: Atrophy or thinning of the muscles surrounding the affected joint due to disuse.
- Joint Deformity: Noticeable changes in the joint's shape or alignment compared to the unaffected side.
- Crepitus: A grinding or crackling sensation felt when moving the joint through its range of motion.
Osteoarthritis Diagnosis Diagnostic Methods
Medical professionals use the osteoarthritis icd 10 codes to formally document the diagnosis during a clinical evaluation.
- Physical Exam: Checking for tenderness, swelling, redness, and flexibility.
- X-rays: Revealing bone spurs and the narrowing of the space between bones in the joint.
- MRI: Providing detailed images of cartilage and soft tissues, though not always necessary for a standard diagnosis.
- Joint Fluid Analysis: Drawing fluid from the joint to rule out gout or infection.
Osteoarthritis Treatment
An effective osteoarthritis treatment plan typically focuses on reducing pain and improving joint function through a variety of non-surgical methods. Common medications include over-the-counter pain relievers and anti-inflammatory drugs to manage daily discomfort. Physical therapy provides custom exercises to strengthen the muscles around the joint and increase the overall range of motion.
Occupational therapy helps patients learn how to perform everyday tasks without putting extra stress on their painful joints. For more persistent pain, doctors may suggest injections such as cortisone or lubrication injections like hyaluronic acid directly into the joint space. In cases requiring severe osteoarthritis treatment, surgical options like joint replacement or osteotomy may be considered to restore mobility when conservative methods fail.
Frequently Asked Questions About Osteoarthritis
What is the best treatment for osteoarthritis?
The best approach is usually a combination of weight management, regular low-impact exercise, and physical therapy tailored to the specific joint involved.
How serious is osteoarthritis?
It is a serious chronic condition because it can lead to permanent joint damage and significant disability if the pain and mobility issues are not managed effectively.
What foods should you avoid if you have osteoarthritis?
You should limit highly processed foods, sugary drinks, and excessive saturated fats, as these can promote inflammation throughout the body.
What are the four stages of osteoarthritis?
The four stages are minor, mild, moderate, and severe, representing the progressive loss of cartilage and the growth of bone spurs within the joint.
Which medical department should be consulted for Osteoarthritis?
You should consult the Rheumatology or Orthopedics departments for a comprehensive diagnosis and long-term management plan for joint health.

 Let Us Call You
Let Us Call You





















































