Testicular cancer is a highly treatable malignancy that develops in the testicles, the two male reproductive glands located inside the scrotum. While this condition is less common than other types of cancer affecting men, it is distinctive because it frequently impacts younger populations. Modern oncology has made significant strides in managing this disease, ensuring that most patients return to their normal lives following a successful recovery path.
What is Testicular Cancer?
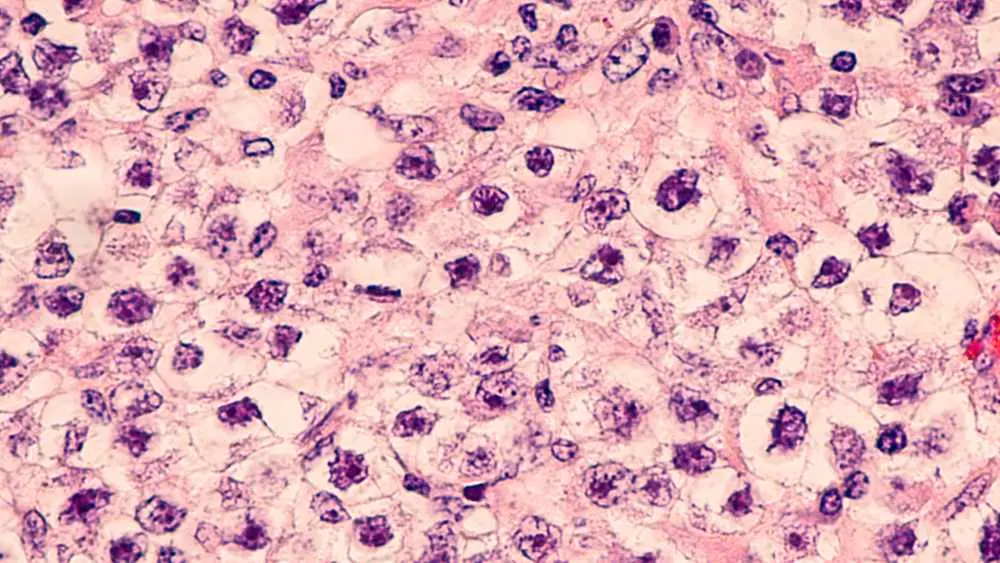
Research into cancer testicular variants shows that this disease primarily starts in the germ cells, which are the cells responsible for producing sperm. There are two main types of these germ cell tumors: seminomas, which tend to grow more slowly and are very sensitive to radiation, and non-seminomas, which are more aggressive and typically occur in younger men. Understanding which cell type is involved is critical for healthcare providers when designing an effective management plan.
What Causes Testicular Cancer?
While doctors are still researching the exact triggers, several testicular cancer causes and risk factors have been identified as significant contributors to cell mutation:
- Cryptorchidism: Having an undescended testicle at birth significantly increases the risk, even if the organ was surgically moved.
- Family History: Having a father or brother who has had the disease increases a man's individual risk profile.
- Age Factors: The disease is most frequently diagnosed in males between the ages of 15 and 45.
- Race and Ethnicity: Statistics show that the condition is more prevalent among white men than men of other races.
Testicular Cancer Symptoms
Patients usually notice testicular cancer symptoms when they feel a change in the physical weight or texture of the scrotum during daily activities. Early detection is often dependent on the patient being aware of what is normal for their body. Common indicators include:
- A small, hard growth on the testicle that usually does not cause immediate pain.
- A persistent feeling of weight or dragging in the lower pelvic area.
- Discomfort or pressure localized in the lower abdomen or the groin.
- A sudden buildup of fluid in the scrotum that causes visible swelling.
Signs Of Testicular Cancer
Clinical signs of testicular cancer can be observed by medical professionals during a physical examination or through changes in hormone-sensitive tissues. During a check-up, a physician looks for specific physiological markers that suggest the presence of a tumor:
- Asymmetry: A noticeable enlargement or change in the shape of one testicle compared to the other.
- Texture Change: A loss of the normal spongy texture, replaced by a firm or irregular surface.
- Breast Tenderness: In rare cases, germ cell tumors secrete hormones that lead to breast enlargement or soreness.
- Swollen Lymph Nodes: Advanced cases may show swelling in the neck or back as the disease travels through the lymphatic system.
Testicular Cancer Diagnostic Methods
Detecting a testicular cancer lump is the initial step in a comprehensive diagnostic process that involves imaging and blood work. Once a mass is suspected, doctors typically order a scrotal ultrasound to determine if the growth is inside or outside the testicle.
Blood tests are also conducted to check for tumor markers such as AFP, HCG, and LDH. Unlike other cancers, a needle biopsy is rarely performed because it risks spreading the cancer; instead, the diagnosis is usually confirmed through the surgical removal of the affected tissue.
Testicular Cancer Treatment
The testicular cancer survival rate is remarkably high compared to many other malignancies, thanks to advances in multi-modal therapy and early detection. Treatment strategies are tailored to the specific type and stage of the disease.
Beyond the initial surgery, patients may undergo chemotherapy to eliminate systemic cells or radiation therapy to target localized areas. Surveillance is also a common approach for early-stage cases, involving regular scans and blood tests to ensure the disease has not returned.
Testicular cancer surgery
Undergoing testicular cancer surgery is often the primary and most critical intervention for both diagnosing and treating the condition. The standard procedure is a radical inguinal orchiectomy, where the entire testicle is removed through an incision in the groin.
In some instances, a more complex operation called a retroperitoneal lymph node dissection (RPLND) is required to remove lymph nodes in the back. These procedures are highly refined to minimize impact on future fertility and overall health.
Which medical department should be consulted for testicular cancer?
You should initially consult a urology department, as urologists are the specialists trained to manage the male reproductive system and perform the necessary surgical procedures. If the cancer is confirmed, you may also work with a medical oncologist to coordinate further treatments like chemotherapy.

 Let Us Call You
Let Us Call You






































