Diabetes type 2 is a chronic health condition that occurs when the body does not process blood sugar correctly, leading to elevated glucose levels. Unlike other forms of the disease, this condition is primarily characterized by insulin resistance or a relative lack of insulin. If left unmanaged, it can lead to serious complications such as heart disease, vision loss, and kidney damage.
What is The Type 2 Diabetes?
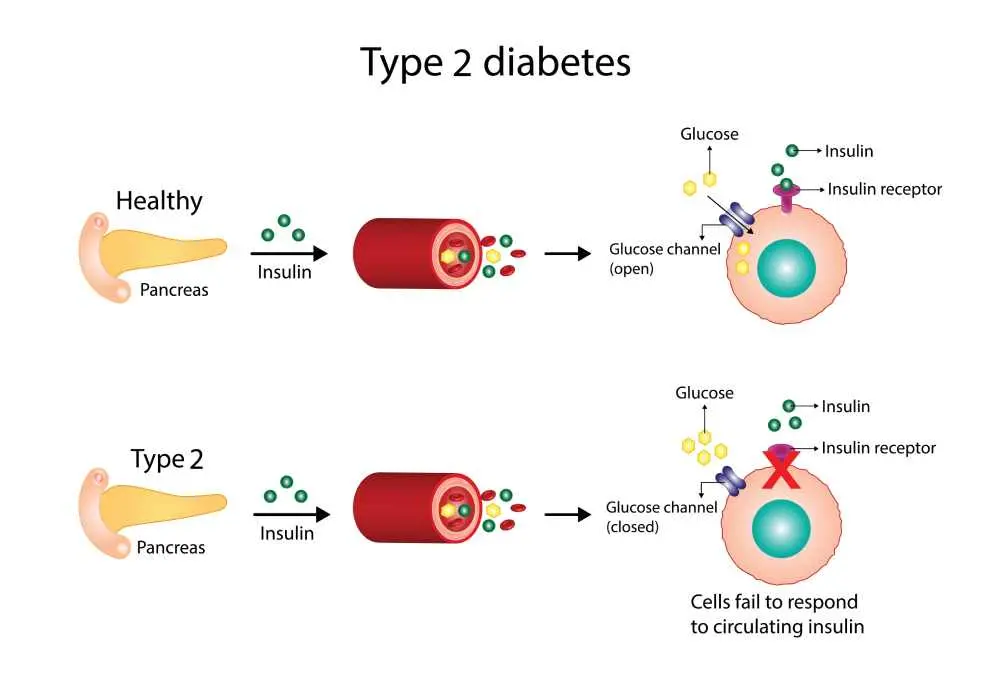
The clinical condition known as type 2 diabetes mellitus describes a metabolic disorder where the body’s cells fail to respond to insulin, preventing glucose from entering the cells for energy. Over time, the pancreas becomes unable to produce enough insulin to overcome this resistance, causing sugar to build up in the bloodstream. While it was once considered a disease of adulthood, it is increasingly diagnosed in younger populations due to lifestyle shifts.
What Causes Type 2 Diabetes?
Developing type 2 diabetes is usually the result of a complex interplay between a person's genetic makeup and daily lifestyle choices. While being overweight and physically inactive are the leading environmental drivers, the biological cause is rooted in the body's inability to use the hormone insulin effectively. This dysfunction prevents the liver and muscles from absorbing sugar, which eventually exhausts the insulin-producing capacity of the pancreas.
- Insulin resistance
- Weight factors
- Genetic history
- Inactivity
Type 2 Diabetes Symptoms
Recognizing type 2 diabetes symptoms is often difficult because they tend to develop very slowly over many years. Many people live with the condition for a long time without noticing any significant changes in their health. However, as blood sugar remains high, several classic indicators begin to emerge:
- Frequent dehydration as the body tries to flush out excess sugar.
- Needing to urinate more often, especially during the night.
- Feeling constantly tired because your cells aren't getting the energy they need.
- Persistent hunger even after eating, as sugar stays in the blood instead of feeding cells.
Signs of Type 2 Diabetes
Early signs of type 2 diabetes may also include physical changes that are not immediately linked to blood sugar levels. These red flags often involve the body’s ability to heal or changes in the appearance of the skin. If you notice these issues, it is important to seek medical advice:
- Cuts and bruises that take an unusually long time to heal.
- Dark, velvety patches in body folds, such as the neck or armpits.
- High sugar levels causing fluid to be pulled from the lenses of the eyes.
- A pins-and-needles sensation in the hands or feet caused by nerve damage.
Type 2 Diabetes Treatment
A successful type 2 diabetes treatment plan focuses on stabilizing blood sugar levels through a combination of lifestyle modifications and, if necessary, medical intervention. The primary goal is to prevent long-term damage to the organs by keeping glucose within a target range. Effective management typically involves:
- Healthy Eating: Consuming high-fiber, low-fat foods while limiting refined carbs and sugars.
- Regular Exercise: Engaging in physical activity to help the body use insulin more efficiently.
- Weight Management: Losing even a small percentage of body weight can significantly improve blood sugar.
- Medication: Oral drugs like Metformin or injectable therapies to help manage glucose production.
- Monitoring: Checking blood sugar levels regularly to track the effectiveness of the treatment.
Frequently Asked Questions About Type 2 Diabetes
What are the 4 stages of type 2 diabetes?
The disease typically progresses through insulin resistance, the onset of prediabetes, the official clinical diagnosis, and finally the development of chronic complications if blood sugar remains uncontrolled.
Can type 2 diabetes be reversed permanently?
While the term remission is more accurate than reversal, many people can achieve and maintain normal blood sugar levels through significant weight loss and permanent lifestyle changes.
What's the difference between type 1 and 2 diabetes?
Type 1 is an autoimmune condition where the body stops producing insulin entirely, while type 2 is a metabolic disorder where the body becomes resistant to the insulin it does produce.
Is type 2 diabetes genetic?
There is a strong genetic link to the disease, meaning you are at a higher risk if a parent or sibling has it, though lifestyle choices often determine if the condition develops.
Which medical department should be consulted for Type 2 Diabetes?
Patients should visit the Endocrinology department, where specialists focus on hormone-related disorders and the management of metabolic conditions like high blood sugar.

 Let Us Call You
Let Us Call You

























