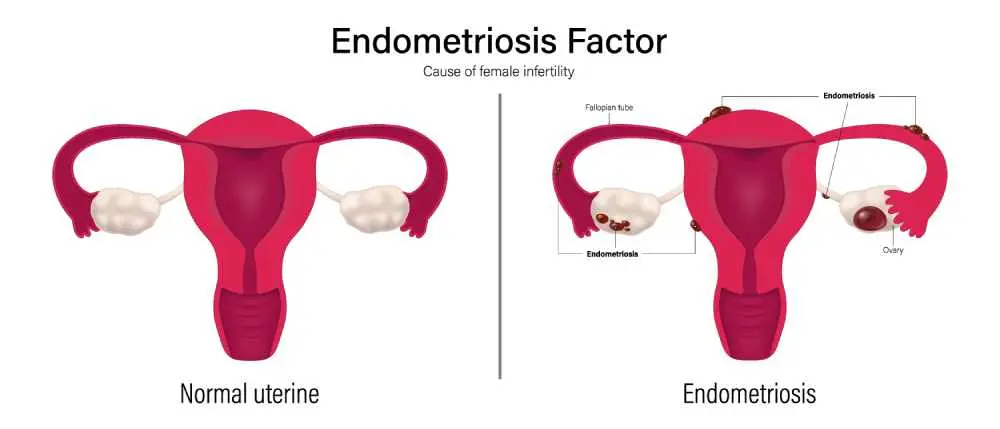
The endometriosis meaning refers to a painful disorder where tissue similar to the lining inside the uterus—the endometrium—grows outside the uterine cavity. This misplaced tissue continues to act as it normally would: it thickens, breaks down, and bleeds with each menstrual cycle. Because this tissue has no way to exit the body, it becomes trapped, leading to inflammation, scar tissue formation, and potentially severe pelvic pain. While it most commonly involves the ovaries, fallopian tubes, and the tissue lining the pelvis, it can occasionally spread beyond the pelvic organs in more complex cases.
What is Endometriosis?
Clinicians often use the endometriosis icd 10 code N80 to classify this chronic condition where endometrial-like stroma and glands develop in extrauterine sites. When this happens, the surrounding tissue can become irritated, eventually developing fibrous bands of scar tissue called adhesions. In advanced cases, such as stage 4 endometriosis, the condition can involve deep implants and large cysts on the ovaries, significantly impacting a person’s quality of life and reproductive health.
What Causes Endometriosis?
While the exact endometriosis causes remain a subject of ongoing research, several theories suggest that retrograde menstruation plays a significant role in its development.
- Retrograde Menstruation: Menstrual blood containing endometrial cells flows back through the fallopian tubes into the pelvic cavity.
- Cell Transformation: Hormones or immune factors may transform peritoneal cells or embryonic cells into endometrial-like cells.
- Surgical Scar Implantation: Endometrial cells may attach to a surgical incision, such as after a C-section or hysterectomy.
- Immune System Disorders: A problem with the immune system may make the body unable to recognize and destroy endometrial-like tissue growing outside the uterus.
- Hormonal Influence: High levels of estrogen are known to fuel the growth of the condition.
Endometriosis Symptoms
The most prevalent endometriosis symptoms involve pelvic pain, often associated with menstrual periods, which is frequently far more severe than typical cramping.
- Dysmenorrhea: Painful periods that may begin several days before and extend several days into the menses.
- Pain with Intercourse: Discomfort during or after sex is a common indicator of the condition.
- Painful Bowel Movements: Discomfort experienced during urination or defecation, particularly during a period.
- Excessive Bleeding: Experiencing heavy menstrual periods or bleeding between cycles (intermenstrual bleeding).
- Infertility: For some, the condition is first discovered during a consultation for difficulty conceiving.
Signs of Endometriosis
Specific physical signs of endometriosis may be identified during a pelvic exam, such as the presence of palpable nodules or fixed pelvic organs.
- Small, firm lumps that can be felt in the pelvic area during a manual examination.
- Pelvic organs (like the uterus or ovaries) that do not move freely because they are stuck together by scar tissue (adhesions).
- Unusual pain or sensitivity in specific spots during a doctor's physical check-up.
- Fluid-filled cysts on the ovaries that can be felt or seen on imaging, often containing dark, old blood.
- Visible, persistent abdominal bloating that is often painful and worsens during the menstrual cycle.
- Persistent exhaustion and low energy levels that do not improve with sleep or rest.
Endometriosis Diagnostic Methods
Advanced endometriosis radiology techniques are essential for mapping the location and extent of tissue growth before determining a management plan.
- Endometriosis Ultrasound: Often the first imaging step, using sound waves to create pictures of the reproductive organs and identify cysts.
- Endometriosis MRI: This provides high-resolution images that help surgeons plan for complex cases by showing the exact size and location of implants.
- Endometriosis CT: While less common for primary diagnosis, a endometriosis CT may be used to rule out other causes of abdominal pain or complications.
- Laparoscopy: A minor surgical procedure that allows a doctor to view the pelvic cavity directly; this is the only way to confirm a diagnosis through endometriosis pathology samples.
Endometriosis Treatment
A customized endometriosis treatment plan typically focuses on managing pain levels and addressing fertility concerns through medication or therapy. Hormonal therapies, such as birth control pills, progestin therapy, or Gn-RH agonists, are frequently used to slow the growth of endometrial tissue and reduce symptoms. For many patients, nonsteroidal anti-inflammatory drugs (NSAIDs) provide relief from the intense cramping associated with the menstrual cycle.
Endometriosis Surgery
In cases where conservative measures fail, endometriosis surgery is performed to remove as much of the ectopic tissue as possible while preserving the uterus and ovaries. This is typically done via laparoscopy, where a surgeon uses specialized tools to excise or ablate the growths. In severe scenarios where a patient no longer wishes to conceive, a hysterectomy might be considered a last resort. Modern surgical techniques aim to restore normal anatomy and improve the chances of natural conception.
Frequently Asked Questions About Endometriosis
How is endometriosis diagnosed?
The condition is initially suspected based on symptoms and imaging but can only be definitively diagnosed through a surgical procedure called a laparoscopy.
Is endometriosis genetic?
Research suggests a strong genetic link, as you are significantly more likely to develop the condition if a close relative, such as a mother or sister, has it.
How to know if you have endometriosis?
You may have it if you experience debilitating period pain, chronic pelvic discomfort, or pain during intercourse that interferes with your daily activities.
How to test for endometriosis?
Testing typically involves a pelvic exam followed by imaging like an ultrasound or MRI, though a biopsy during laparoscopy is the final confirmatory test.
Can you get pregnant with endometriosis?
Many people with the condition can still get pregnant, although it may be more difficult, and some may require fertility treatments or surgery to conceive.
Which medical department should be consulted for Endometriosis?
Patients should consult the Gynecology department, specifically a specialist who focuses on reproductive medicine or chronic pelvic pain disorders.

 Let Us Call You
Let Us Call You











































