Aortic valve disease is used to refer to disorders that affect the proper dilation of the aortic valve (stenosis) or constriction of the aortic valve (regurgitation), interfering with the forward blood flow between the left ventricle and the aorta. It can silently develop over several years and then either have exertional symptoms or heart failure manifestations. Strong emphasis is placed on early identification and risk-based follow-up since the disease at advanced stages leads to a huge morbidity and mortality. Management spans between the surveillance and medical optimization intervention, to valve repair or replacement, including catheter-based intervention.
What is Aortic Valve Disease?
Aortic valve disease is a health condition whereby the aortic valve becomes obstructed (aortic stenosis) or leaky (aortic regurgitation), or both. These abnormalities add to afterload or result in volume overload, resulting both in ventricular remodeling and symptoms with time. Primary types include:
- Aortic stenosis (AS): Narrowing which tends to become progressed, usually due to calcific or congenital degeneration, or owing to bicuspid valve.
- Aortic regurgitation (AR): This is the result of incomplete leaflet coaptation due to leaflet disease (e.g., bicuspid, rheumatic) or dilation of the aortic root.
Symptoms of Aortic Valve Disease
The symptoms of the aortic valve disease regularly manifest themselves during exercise and do not always appear in the initial stages. The common characteristics are low exercise capacity and symptoms of heart failure during disease progress. Early assessment is justified in case of red-flag symptoms.
Symptoms of the aortic valve disease:
- Vigorous dyspnea and lack of strength
- Angina, which exhibits pressure (activity related chest pain)
- Lightheadedness or syncope
- Palpitations, heart arrhythmia
- Peripheral edema (ankles/feet), fatigue with or without exertion
Aortic Valve Disease Causes
Valve disease in the aorta is due to degenerative, congenital, inflammatory or systemic mechanisms. Aortic valve disease causes:
- Valve degeneration in old age which is calcific in nature
- Bicuspid aortic valve as a result of congenital defects with early stenosis or regurgitation
- Leaflet scarring/retraction rheumatic heart disease
- Aortic root disease
- Systemic risk: hypertension, dyslipidemia, diabetes, chronic kidney disease (accelerated calcification/progression)
How is Aortic Valve Disease Diagnosed?
Diagnosis is a combination of clinical and imaging diagnosis that characterizes severity and determines intervention timing
- Physical examination and cardiac examination
- Transthoracic echocardiography: the initial examination in an attempt to measure gradients, valve area, the severity of regurgitation and the ventricular function
- It may be stress testing (exercise or pharmacologic) in selected asymptomatic severe cases
- Anatomy, calcium burden, or root pathology Cardiac CT/MRI; cardiac catheterization when noninvasive data are ambiguous or planning TAVI is required
- ECG and general laboratory tests to assess comorbidities and end-organ involvement
How is Aortic Valve Disease Treated?
Individualization of the treatment depends on the type of lesion (AS vs AR), severity, symptoms and the risk of surgery. Management pillars:
- Active follow-up with periodic echocardiography of mild-moderate disease
- Medical treatment to contain comorbidities (e.g. blood pressure), to treat arrhythmias and to treat congestion with diuretics- note medicines do not treat mechanical valve disease
Indication of valve intervention:
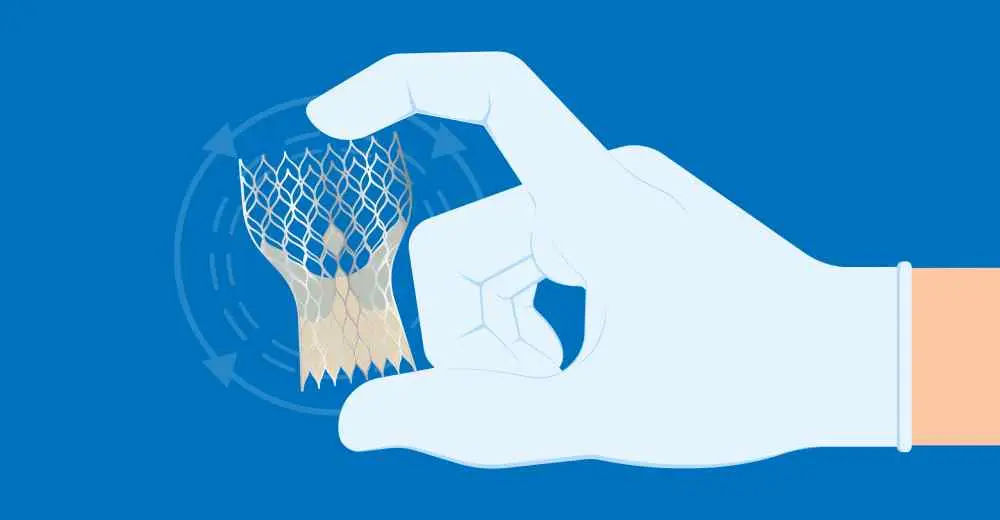
- TAVI/TAVR in a large number of patients with severe AS (in particular, more surgical risk; broadening criteria according to the guidelines)
- Surgical aortic valve replacement (SAVR) in appropriate candidates; aortic valve repair in appropriate AR or root operations.
- Bridge or palliative option Balloon valvuloplasty in selected AS cases.
Risk Factors for Aortic Valve Disease
Risk is also more likely to go up with age and certain structural or systemic conditions. Key factors:
- Later age (progressive calcification)
- Deviant valves (congenital e.g. bicuspid valve)
- History of rheumatic fever
- Hypertension, dyslipidemia, diabetes, chronic kidney disease
- Inflammatory/endocarditic processes
This content is for informational purposes only and is not a substitute for medical advice. If you’re experiencing any of these symptoms, please contact us for professional help.
Frequently Asked Questions About Aortic Valve Disease
Is aortic valve disease serious?
Severe untreated disease particularly aortic stenosis may result in syncope, heart failure and elevated mortality. Prompt evaluation and where necessary, valve repair enhance the results.
What are the stages of aortic valve disease?
Timing of intervention depends on the clinical staging of symptoms and ventricular functioning (e.g., ACC/AHA stages C1 -C2 and D) and determines the timing of intervention.
Can you repair an aortic valve without surgery?
In the severe case of aortic stenosis, many patients have TAVI/TAVR, a catheter-based (non-open-heart) replacement; surgery rarely involves a true repair of AS. Temporary relief could be provided with balloon valvuloplasty.
Is aortic disease a disability?
The disease of aortic valves is potentially debilitating, and in severe cases might be considered disabling in relation to the symptom burden, the ejection fraction, and national standards. The choice is case-oriented and depends on objective clinical data and outcome to treatment.
Which department should I visit for Aortic Valve Disease?
Patients with Aortic Valve Disease should visit the Cardiology Department to be evaluated by a heart specialist. In advanced cases, the cardiologist may refer the patient to Cardiovascular Surgery for further treatment.

 Let Us Call You
Let Us Call You

















































