Myasthenia Gravis is a long term autoimmune disease of the neuromuscular system leading to weakness of voluntary muscles. It is a condition that arises when a breakdown of communication between nerves and muscle occurs as a result of an attack by the immune system. The condition mostly takes place in the eyes, face, throat, and limbs causing the muscles to be weakly varying. Although it is incurable, it can be controlled by the modern treatment which allows most of the people to control their symptoms.
What is Myasthenia Gravis?
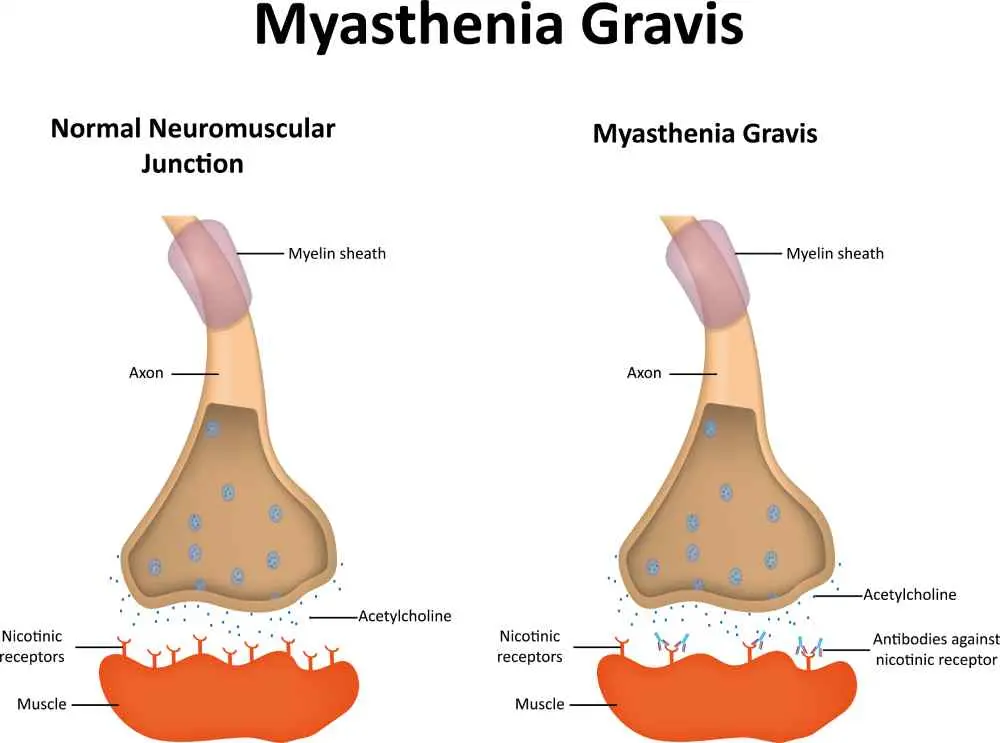
Myasthenia Gravis is an autoimmune disease that interferes with the conduction of nerve impulses to the muscles. This leads to the development of antibodies by the immune system to obstruct or destroy acetylcholine receptors in the neuromuscular junction. This prevents proper contraction of muscles resulting in fatigue and weakness. People of all ages may be affected by the condition but predominantly women who are under 40 years old and men, those above 60 years.
Myasthenia Gravis Symptoms
The symptoms of MG tend to manifest slowly and to differ in their intensity during the day. The weakness of the muscles is usually an increase with activity and a decrease with rest. The symptoms are either localized (ocular) or generalized, which is in many muscle groups.
Common symptoms include:
- Drooping eyelids (ptosis)
- Double vision (diplopia)
- Problems with speech or with swallowing
- Arm, hand, leg or neck weakness
- Difficulty breathing or shortness of breath (in extreme cases)
- Weakness in facial muscles with restriction of expression
Causes of Myasthenia Gravis
Myasthenia Gravis is mainly induced by an autoimmune process which disrupts nerve-to-muscle contact. Their attack is directed at the acetylcholine receptors or related proteins of the neuromuscular junction and causes the weakening of signals and muscle contraction.
Myasthenia Gravis causes include:
- Autoimmune activity: The immune responds by attacking the acetylcholine receptors.
- Abnormalities of the thymus glands: Thymic hyperplasia or thymoma is a frequent phenomenon in MG.
- Genetic predisposition: There are some people who are born with the variation in their immune system as an increase in risk factor.
- Medication triggers: Some antibiotics and beta blockers may aggravate the symptoms.
Risk Factors for Myasthenia Gravis
Myasthenia Gravis risk factors affect the development and severity of the disease. Although it can occur to anyone, there are factors that increase the chances of occurrence.
Key risk factors include:
- Ages: The most frequent victims are women younger than 40 years and men older than 60 years.
- Autoimmune diseases: Individuals with lupus, rheumatoid arthritis or thyroid disease are more prone.
- Genetics: There can be family history of autoimmune diseases.
- Thymus gland issues: There is the potential of increased susceptibility due to abnormal thymus structure or functioning.
Diagnosis of Myasthenia Gravis
Diagnosis of myasthenia gravis is performed by clinical examination, neurological investigation, and laboratory research. Doctors seek muscle fatigue which gets aggravated by activity and also gets better with rest.
Common diagnostic methods:
- Physical and neurological review: Examine muscle strength and reflexes.
- Blood tests: Identify anti-AChR or anti-MuSK antibodies.
- Electromyography (EMG): Assessment of muscle response to repetitive nerve stimulation.
- Imaging (CT/MRI): Assesses thymus gland on abnormalities.
- Edrophonium (Tensilon) test: Temporarily enhances the strength of the muscles on diagnostic confirmation.
Treatment Options for Myasthenia Gravis
Myasthenia Gravis Myasthenia Gravis can be treated by enhancing muscle activity and managing the autoimmune response. Treatment is based on the severity and the muscles affected.
Common treatment options:
- Anticholinesterase drugs: Pyridostigmine enhances neurono-muscular communication.
- Corticosteroids and immunosuppressants: Prednisone, azathioprine and cyclosporine suppress the immune response.
- Plasma exchange (plasmadialysis): Removes toxic antibodies in the blood.
- Intravenous immunoglobulin (IVIG): Temporarily suppresses the attack of the immune.
- Thymectomy: The thymus gland is removed with surgical means so as to enhance long-term results.
- Lifestyle management: Proper sleep, alleviation of stress and prevention of infection help to control it.
This content is for informational purposes only and should not be considered medical advice. If you are experiencing any of the mentioned symptoms, please fill out the form to contact us for professional support.
Frequently Asked Questions About Myasthenia Gravis
What are the risk factors for developing Myasthenia Gravis?
Myasthenia Gravis is more likely to occur in old age, females, and with the presence of other autoimmune conditions. There are also abnormalities in the thymus glands and hereditary predispositions.
How is Myasthenia Gravis diagnosed?
Diagnosis Diagnosis is done by blood antibody, electromyography (EMG) or imaging of thymus gland. Such tests approve damaged nerve-muscle communication.
Which department should you visit for Myasthenia Gravis?
In the early stages, Myasthenia Gravis may be evaluated by the ophthalmology department due to symptoms like drooping eyelids. However, after diagnosis, since it is a neurological condition, patients are referred to the neurology department for further assessment and treatment.
What is the pathophysiology of Myasthenia Gravis?
It is caused by the antibodies which attack acetylcholine receptors at the neuromuscular junction and this prevents normal muscle contraction resulting in weakness.
What medications are used for Myasthenia Gravis?
Commonly used drugs include anticholinesterase medications such as pyridostigmine, and immunosuppressants such as prednisone to help with the symptoms and the immune activity.
What is ocular Myasthenia Gravis and how does it differ from generalized Myasthenia Gravis?
Ocular Myasthenia Gravis is also specific to the eye muscles resulting into drooping eyelids or double vision whilst the generalized form affects the muscles of the body in a number of ways.
What is generalized Myasthenia Gravis and how does it differ from ocular Myasthenia Gravis?
Generalized Myasthenia Gravis is an extrapyramidal disease, which involves facial, limb and respiratory muscles in addition to eye movement ocular MG.
What is the ICD-10 code for Myasthenia Gravis?
Myasthenia Gravis is classified under the ICD-10 code of G70.0 used in the medical records and billing classification.
Can Myasthenia Gravis be cured or what is the prognosis?
It is incurable but the symptoms can be treated. Through appropriate medical care and lifestyle changes, many patients lead full and active lives.

 Let Us Call You
Let Us Call You






























