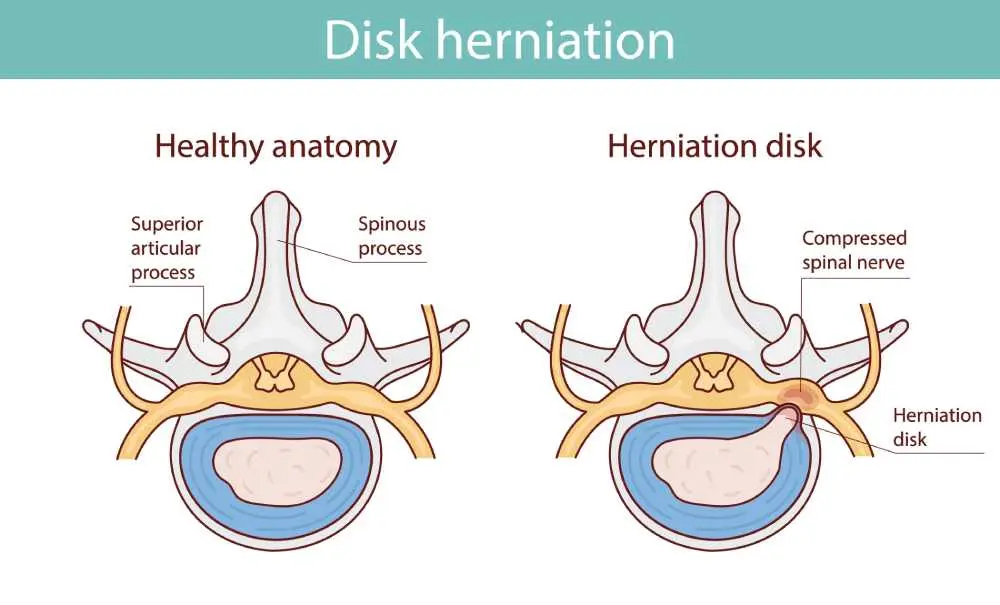
A herniated disc refers to a problem with one of the rubbery cushions (discs) that sit between the individual bones (vertebrae) that stack to make up your spine. These spinal discs act as shock absorbers, but when the soft, jelly-like center pushes out through a tear in the tougher exterior, it can irritate nearby nerves.
This condition can occur anywhere along the spine, leading to varying degrees of discomfort, numbness, or weakness in the limbs. Understanding the mechanics of the spine is essential for managing the condition and preventing further injury.
What is Herniated Disc?
The clinical term lumbar disc herniation describes a specific instance where the displacement of disc material occurs in the lower back region of the spine. While the spine is designed for flexibility and strength, repetitive stress or sudden trauma can cause the inner nucleus to slip out of its protective casing.
This displacement often leads to inflammation and pressure on the spinal nerves, causing the classic symptoms associated with slipped or ruptured discs. Though it most commonly affects the lower back, it remains a significant cause of spinal pain globally.
What is the Cause of Herniated Disc?
A disc herniation is most often the result of gradual, aging-related wear and tear called disc degeneration.
- Disc Degeneration: As people age, spinal discs lose water content, making them less flexible and prone to tearing.
- Improper Lifting: Using back muscles instead of leg muscles to lift heavy objects can cause acute injury.
- Repetitive Strain: Constant twisting or bending can weaken the outer ring of the disc.
- Traumatic Events: In rarer cases, a fall or a blow to the back can shift disc material out of place.
Herniated Disc Symptoms
The most common herniated disc symptoms include sharp, radiating pain that travels from the spine into the extremities.
- Discomfort that shoots from the spine into the buttocks, legs, or arms.
- Sensations ranging from a dull ache to an intense, electric-shock feeling.
- Weakness in the affected area which can cause stumbling or difficulty lifting items.
- Some individuals may have no symptoms, with the condition only appearing on unrelated imaging.
Signs of Herniated Disc
If you are experiencing a herniated disc in neck, the signs typically involve sudden shooting pain and neurological changes.
- Shooting Pain: Sharp pain in the shoulder or arm triggered by coughing or sneezing.
- Paresthesia: A "pins and needles" tingling sensation or numbness in the fingers and hands.
- Lower Spine Indicators: Intense pain localized in the calf or foot for lower back herniations.
- Nerve Compression: Signs indicating a compressed nerve root that requires professional medical evaluation.
Herniated Disc Diagnosis
To accurately identify herniated discs, physicians usually begin with a physical exam to check for tenderness, muscle strength, and walking ability. During the neurological portion of the exam, the doctor may test your reflexes and your ability to feel light touches or vibrations.
Imaging tests play a vital role in confirming the diagnosis; an MRI is the most common tool used to pinpoint the exact location of the herniated disc and see which nerves are affected. In some instances, X-rays are used to rule out other causes of back pain like fractures or tumors.
Herniated Disc Treatment
A herniated disc lower back is frequently managed through conservative methods such as physical therapy, rest, and anti-inflammatory medications. The goal of treatment is to relieve pain and restore mobility while allowing the body time to naturally resorb the protruding disc material.
Patients are often encouraged to modify their activities to avoid movements that aggravate the nerve, such as heavy lifting or prolonged sitting. If the pain persists after several weeks of conservative care, doctors may suggest corticosteroid injections to reduce inflammation around the nerve.
Herniated Disc Surgery
While most cases resolve without it, cervical disc herniation or severe lumbar cases may eventually require surgical intervention if the nerve compression causes significant weakness or loss of bladder control.
The most common procedure is a microdiscectomy, where the surgeon removes only the portion of the disc that is pressing on the nerve. Another option is a laminectomy, which involves removing a small piece of bone to create more space for the spinal cord. Most patients experience a significant reduction in leg or arm pain shortly after these minimally invasive procedures.
Frequently Asked Questions About Herniated Disc
Signs herniated disc is healing?
You will notice a gradual reduction in radiating limb pain and an improvement in muscle strength and flexibility.
How to fix a herniated disc?
Most cases are fixed through a combination of physical therapy, pain management, and specific strengthening exercises for the core muscles.
Will a herniated disc heal on its own?
Yes, in many cases the body eventually reabsorbs the displaced disc material through a natural process of inflammation and shrinkage.
Is a herniated disc serious?
It can be serious if it causes severe nerve compression, leading to permanent weakness or loss of bowel and bladder function.
What does a herniated disc feel like?
It typically feels like a sharp, burning, or electric sensation that travels from the spine into the extremities, often accompanied by numbness.
Which medical department should be consulted for Herniated Disc?
You should consult the Orthopedics or Neurosurgery departments, though a Physical Therapy and Rehabilitation specialist can also provide non-surgical care.

 Let Us Call You
Let Us Call You
























































