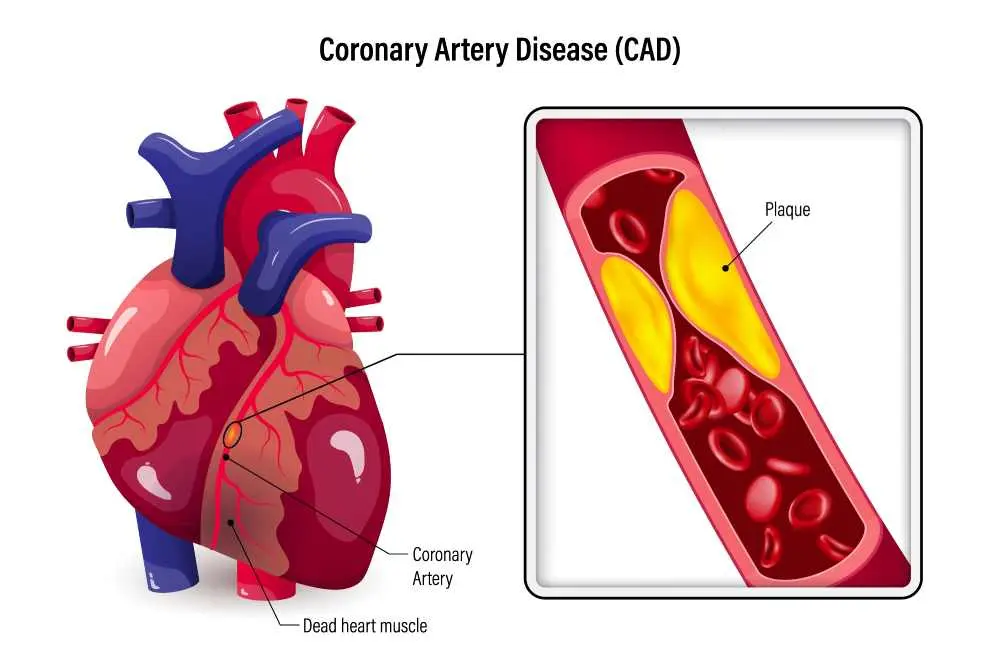
Coronary artery disease occurs when the major blood vessels that supply the heart become damaged or diseased. These arteries are responsible for delivering oxygen-rich blood and essential nutrients to the heart muscle. When cholesterol-containing deposits, known as plaque, build up in your arteries and cause inflammation, the vessels narrow, decreasing blood flow to the heart. This process can take decades to develop, often going unnoticed until a significant blockage or a heart attack occurs, making preventive care and lifestyle management crucial for long-term cardiovascular health.
What is Coronary Artery Disease?
In the ICD-10 classification system, coronary artery disease is categorized as a chronic narrowing of the arteries that leads to myocardial ischemia. Essentially, it is a condition where the heart muscle does not receive enough blood to function at its peak, especially during physical exertion or stress. Over time, the reduced blood flow can weaken the heart muscle, leading to heart failure or dangerous rhythm disturbances that require immediate medical intervention.
Types of Coronary Artery Disease
While many people refer to it generally, ischaemic coronary artery disease can manifest in several distinct clinical forms depending on how the blockage develops. Obstructive coronary artery disease involves arteries that are physically narrowed by at least 50%, whereas non-obstructive disease involves smaller plaques or dysfunction in the smaller vessels. Another specific type is spontaneous coronary artery dissection (SCAD), where a tear forms inside an artery, potentially blocking blood flow without any prior plaque buildup.
Stages of Coronary Artery Disease
The progression of coronary artery disease treatment often depends on which of the four stages the patient is currently experiencing as the arteries change over time.
- Fatty Streak Formation: The earliest stage where microscopic deposits of cholesterol begin to accumulate in the inner lining of the artery walls.
- Plaque Progression: The fatty streaks grow and harden into fibrous plaques, beginning to narrow the space available for blood to flow.
- Complicated Lesion: The plaque becomes unstable and may develop cracks or small tears, which can trigger the formation of blood clots.
- Total Occlusion: The artery becomes completely blocked by a combination of plaque and clots, typically resulting in a heart attack or severe tissue damage.
Coronary Artery Disease Causes
The primary coronary artery disease symptoms often stem from atherosclerosis, a condition where plaque builds up and hardens over many years.
- High Cholesterol: Elevated levels of LDL (bad) cholesterol contribute to the formation of plaques.
- Hypertension: High blood pressure can damage the inner lining of the arteries, making them more susceptible to deposits.
- Smoking: Chemicals in tobacco damage blood vessels and increase the rate of plaque accumulation.
- Diabetes: High blood sugar levels increase the risk of inflammation and vessel damage.
- Sedentary Lifestyle: A lack of physical activity is linked to obesity and other heart-related risks.
- Unhealthy Diet: Diets high in saturated fats and trans fats contribute directly to arterial narrowing.
Coronary Artery Disease Symptoms
Identifying early coronary artery disease symptoms is vital because the condition often progresses silently for many years.
- Angina
- Shortness of breath
- Fatigue
- Nausea
- Pain in extremities
Signs of Coronary Artery Disease
Recognizable signs of coronary artery disease often appear during physical examinations and clinical tests, indicating that the heart is working harder than it should.
- Heart Murmurs: Unusual sounds detected during a physical exam that suggest turbulent blood flow or valve stress.
- Irregular Pulse: A heartbeat that is too rapid or inconsistent, indicating the heart muscle is not receiving enough oxygen.
- Peripheral Edema: Visible swelling in the ankles, feet, or legs caused by the heart's decreased ability to pump blood effectively.
- Xanthomas: Small, yellowish fatty deposits under the skin, which can be a clinical sign of the high cholesterol driving arterial blockage.
- Arcus Senilis: A grey or white ring around the cornea of the eye, sometimes associated with advanced lipid buildup in the body.
Coronary Artery Disease Diagnosis
Determining the appropriate coronary artery disease treatment requires a thorough diagnostic process to map the extent of arterial blockages.
- Electrocardiogram (ECG): Measures electrical activity to see if the heart is under stress.
- Echocardiogram: Uses sound waves to produce images of the heart's structure and pumping power.
- Stress Testing: Monitoring heart function while the patient walks on a treadmill.
- Cardiac Catheterization: Inserting a thin tube into the arteries to inject dye and view blockages on an X-ray.
- CT Scan: Creates detailed cross-sectional images of the heart to check for calcium deposits.
Coronary Artery Disease Treatment
Effective coronary artery disease treatment usually involves a combination of medication, lifestyle changes, and potentially invasive procedures to restore blood flow. Doctors typically prescribe statins to lower cholesterol, beta-blockers to reduce heart rate, and aspirin to prevent dangerous blood clots. For more severe cases, angioplasty and stenting are used to physically open narrowed vessels, while coronary artery bypass grafting (CABG) surgery creates a new path for blood to flow around blocked segments.
Frequently Asked Questions About Coronary Artery Disease
What are 5 symptoms of coronary artery disease?
The most common indicators include chest pain known as angina, shortness of breath during exercise, extreme fatigue, pain radiating to the jaw or neck, and a fluttering sensation in the chest.
What is the coronary artery disease?
It is a condition where the major blood vessels supplying the heart become narrowed or blocked by plaque, limiting the amount of oxygen and nutrients reaching the heart muscle.
What is the survival rate for coronary artery disease?
With modern advancements in medicine and early intervention, the majority of patients can manage the condition effectively and live for decades after their initial diagnosis.
What happens if you have coronary artery disease?
If left untreated, the heart muscle may weaken over time, leading to heart failure, or a plaque may rupture, causing a blood clot that results in a heart attack.
Which medical department should be consulted for Coronary Artery Disease?
Patients should seek consultation from the Cardiology department, where specialists can perform the necessary diagnostic tests and develop a personalized heart health plan.

 Let Us Call You
Let Us Call You







































